Monday, March 13th:
Theo woke up Monday morning with oxygen levels in the low 80s. We decided not to wait until his 10:15 AM appointment and headed to Ottawa as soon as we were all ready. While we were driving I called the Pediatrician and told him that we couldn’t wait until 10:15 AM for the appointment and that we were taking Theo straight to the ER at the OSF St Elizabeth. He told us to come to the office first and that way we can avoid an ER visit. We saw Dr Dave and he listened to Theo’s chest. He knew right away that it was likely another case of pneumonia. They sent us over to the hospital and Theo was put in a room on the 4th floor. They started him on the nebulizer and high-frequency chest wall oscillation therapy with an actual vest. Theo’s oxygen was 75 when we got to his room, so they started him on oxygen immediately.
They then took Theo downstairs (Josh held him in a wheelchair) to get him an x-ray. The x-ray confirmed that he had either pneumonia or a collapsed left lung (they look similar in an x-ray). They couldn’t keep Theo’s oxygen levels high enough, so they put him on two oxygen machines at 100%.
I called Lurie’t to let them know Theo was admitted and we definitely need to cancel surgery. They were sad that Theo was sick and asked me to let them know when he was feeling better.
I also got a call from Make A Wish! We had submitted our application back in November and we finally heard from them! YAY! I told the nice lady on the phone that it wasn’t a good time to chat, but I will call her back when things calm down.
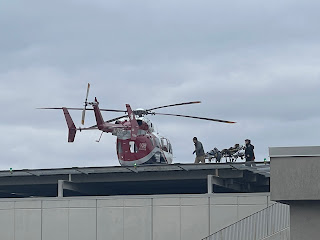
Even with two oxygen machines going at 100%, they could barely keep his oxygen levels in the 90s. Dr Dave came to Theo’s room and told us that they were going to send him to the PICU in Peoria. They were going to look into sending him via ambulance, but they aren’t sure that they carry the amount of oxygen that Theo needs. I started packing while the doctors and nurses tried how to figure out how to best transport Theo. After a few more minutes the nurse walked in with a cart and a computer screen. She was chatting with a PICU nurse and doctor in Peoria who needed to see Theo. They asked her a bunch of questions and then said they have a room for Theo. They then decided that Theo would be safer in a helicopter as they have the right equipment that he needs and it would only be a 30 minute ride as opposed to a two hour ambulance ride.
Once the helicopter ride was set up we decided that I should drive back home, pack a few more things, then drive back to pick up Josh in Ottawa, and then we would drive down to Peoria together. I headed home while Josh waited with Theo. After just a few minutes the chopper arrived and took Theo to Peoria.
Josh and I made the two hour long drive to Peoria (it only took Theo 30 minutes). We knew that Theo would be there for a solid two hours before we arrived, but he was in good hands.
When we arrived there were a lot of doctors and nurses in and out of his room. They are concerned about his lungs but also his brain since he is so lethargic. They ordered a CT to check his shunt and they started an EEG.
[Pizza from Sugar for dinner]
They did a full virus panel and it turns out he has Metapneumovirus. They said there is a really nasty strain going around right now that is causing kids to end up in the hospital with a nasty cough and a lot of mucous. They also started a BiPAP to help him breathe better, but they are struggling to get a good seal with an oronasal mask because they don’t have the right size for him.
He has pneumonia in his entire left lung, which was confirmed during another x-ray. They started him on antibiotics out of precaution - they need to wait a few days for the cultures to grow.
[Lungs are not supposed to be white]
Tuesday, March 14th:
Theo slept all night and had no issues. They said his lung doesn’t show much improvement yet so they’re just waiting on the two antibiotics (vancomycin and rocephin) to break up the mucus. Dr. Miller from Neurosurgery stopped by and said the ventricles looked the same and they are not worried about the shunt.
During rounds they said his lung looked slightly better than yesterday, but he is still very tired. Since Neurosurgery doesn’t think there is an issue with ICP, Theo’s tiredness is likely due to the fact that he is trying to breathe with only one lung. They discussed keeping on the BiPAP breathing machine with the oronasal mask for another day, but it wasn't working like they wanted it to so they switched him to a high-flow cannula. The cannnula allows better access to his nose and mouth so they can suction him better. He had a fever spike so they gave him some Tylenol and we are still waiting on blood cultures.
St Judes called and want to do an ultrasound in the PICU since he had to cancel his appointment. I think that is a great idea and they are going to coordinate it!
Dr Sinha (Neurology) came by and said Theo didn’t have any seizures in the night. Just the regular background noise.
Wednesday, March 15th:
The antibiotics started working on Theo and he had a lot of dirty diapers in the night. He got diaper rash and they ordered him some "PICU cream" that should help. They did another x-ray in the early morning.
Theo was happy and actually opened his eyes when Josh showed up this morning (he slept at the hotel last night). Theo is requiring less oxygen to keep his saturation up in the 90's, but the nasal cannula is not able to open up his left lung. The BiPAP machine and oronasal mask did open his lung a little, but once they took it off, the X-rays today showed that it closed up again.
They discussed trying the BiPAP again with the oronasal mask to see if they can open the lung that way. The next step would be to intubate him and use a ventilator to open it up. Luckily, his blood cultures came back negative, but they are worried that there is an infection in the lung. His doctor also mentioned possibly checking his CSF for an infection too. She is going to see if Neurosurgery wants to tap his VP shunt. If they don't think that's a good idea then they will do a spinal tap.
Dr Sinha with Neurology stopped by and even though Theo isn't showing an increase in seizures he wants to increase his Clobazam from 12 mls to 14 mls. They did some bloodwork and it shows that he can tolerate a little more. I don’t understand it because one of the side effects of Clobazam is pneumonia. He also ordered that the EEG be taken off.
That afternoon they did an ultrasound of Theo's chest and abdomen (for St Judes). They said the he left lung isn't collapsed, but totally filled with gunk. So they don't need to inflate it (which is what the BiPAP would do), but they need to clean it out. The oscillating vest helps, but it's not enough. The doctors are discussing sending a scope down to see what is going on and maybe and doing a chest CT.
After the doctors finished their brainstorming session, they came and talked to us. They said we could try the BiPAP again or we could intubate him. We decided that since he didn't have the best luck with the BiPAP we should just skip it and go right to the ventilator. We figured the ventilator was inevitable and we didn't want them to waste time. The doctors agreed and started preparing to intubate Theo. They gave him a dose of fentanyl and another sedative to keep him relaxed. He will be on a low dose of fentanyl the entire time he is intubated.
Josh and I didn't want to watch him be intubated so we went to the "Meditation Room" to wait. OSF St Francis Children's Hospital is a Catholic hospital and they have bibles, crucifixes, and chapels placed all around the hospital. Josh decided to catch up on some light reading while we were waiting for the nurses to come get us.
The nice thing about being intubated is that the ventilator can breath for Theo and they can send a lot of pressure into the lungs. They can also continue with the oscillating treatments, but it will be done internally by the ventilator. If they aren't able to get the gunk out they can have pulmonology perform a "bronchial scrape" and they can try to get the gunk out that way.
Dr Barbara Stewart the pulmonologist stopped by later that night. We talked a lot about Theo’s medical history and her views for his future care. She said they would do a CT scan of his chest and if things don’t get better they would do a scope to get in there and clean out his lungs. The CT will also help diagnose him with any kind of lung issues (like bronchiectasis). She said they would fight to get us equipment like the high frequency oscillating vest, oxygen, an oxygen monitor, suction equipment, nebulizer, cough assist, etc. She said that she would recommend doing the vest twice a day when he’s healthy and four times a day when he’s sick. She also talked about positioning and how he spends too much time on his left side. We will definitely continue to see her once Theo is discharged from the hospital.
Thursday, March 16th:
Theo slept well last night and his morning x-ray showed some improvement. During rounds they said they they can start a slow feed and they’ll talk to Dr Stewart about a CT scan after she looks at the x-ray.
Theo received a nice gift from his bus driver, Ms. Gina, and his bus aid, Ms Karen. They sent him an adorable and soft wolf and a couple balloons. It was very sweet!
Theo's nurse washed Theo's hair and tried to get the sticky stuff from the EEG out of his hair. It helped, but we really won't be able to get the sticky stuff out until we get Theo home and can put a lot of oil in his hair.
Dr Stewart was able to look at the x-ray and she decided to cancel the bronchoscope for now since his lungs seem to be clearing with the help of the IPV (internal oscillation) and the ventilator. But she did notice a small shadow and it looked like Theo's heart was being pushed slightly to the right. They couldn't tell if that was because of the angle the x-ray was taken or because there was excess fluid or air in the cavity around his lungs. They ordered a late night CT stat and Theo was rushed off downstairs.
I waited in his room and after he came back the doctors said that the CT showed everything we already knew like the pneumonia and some fluid around the lungs. But there was no pneumomediastinum and that was the biggest concern.
Friday, March 17th:
Theo had a great night and is a lot more awake this morning. He actually waved at one of the nurses! I gave him a leg massage and he liked that too. He is pushing the nurses and doctors away when he doesn’t want them, which is a good sign.
[Hiding in the bathroom during the x-ray]
Unfortunately Theo tried to pull out his breathing tube (luckily the respiratory therapist was right there so he could grab Theo's hand). Theo had tears rolling down his cheeks, but he didn't make any sound because his vocal cords are paralyzed (they do that on purpose when people are on a ventilator), but I knew he was sad and that broke my heart. They ended up sedating him some more, so he wouldn't try to pull the tube out again.
His bloodwork is showing low levels of potassium, platelets, and hemoglobin. He's not low enough to warrant a transfusion, but he is close. They are also closely monitoring his in and out liquids and they aren't matching up AND the CT scan showed a little extra fluid, so they gave him lasix (a diuretic) to help flush out that extra fluid.
Josh stayed with Theo at the hospital while I made the two hour drive home. I needed to get my allergy shots, run a few errands around town, do some laundry, and workout.
Look at our flowers! Aren't they beautiful?!
Friday night I did a nice workout, did the laundry, had dinner, and went to bed early.
Saturday, March 18th:
The next morning I did a two hour long bike workout and an hour run. It felt good to be active. I'm dreading my triathlon right now, but it's the least of my current worries.
After my workout I headed north to get my allergy shots and then headed south to Peoria.
Josh and Theo had a good night and morning. They did another x-ray and there is improvement, but it's a slow process. You can clearly see the diaphragm on the x-ray, which wasn't visible before. The PICU doctors said they may approach Dr. Stewart and ask her to reconsider the bronchial scrape.
They have been able to wean Theo's PEEP down to 9 and his oxygen is set at 25. Usually they will extubate when oxygen is 21 and PEEP is 6.
Sunday, March 19th:
Theo's respiratory cultures came back negative for growth, so it doesn't look like there's a bacterial infection, just nasty pneumonia.
Theo isn't usually into stuffed animals, but he's been very cuddley with Wolfie!
We all need naps!
Theo wanted to wrestle after Josh woke up from his nap!
This whole hospital stay is just a waiting game. The ventilator is set to 21% oxygen so he currently doesn't need supplemental oxygen and the PEEP is set to 8. They are still working on trying to get that left lung open. It's likely Theo may be on the ventilator for a few more days, so they can really force some air in there and get him cleaned out.
Before bed they decided to drop Theo's PEEP to 7 and see how he does. They also want to continue his antibiotics for two more days. Ugh! He already has diarrhea and awful diaper rash. But at least he is improving!






































No comments:
Post a Comment